Your employee was exposed to measles. Now what?
Latest measles case counts, plus bird flu costs to dairy industry, flu strains for fall, and what to do if an employee has backyard chickens.
Bird Flu News:
- A non-peer-reviewed preprint study indicates that cows can infect pigs with H5N1, but not spread between them. (CIDRAP)
- Scientists are closely watching a genetic mutation that originated in a California dairy cow herd that could allow for easier mammalian transmission and more severe disease. (LA Times)
- H5N1 is spreading rapidly through Antarctica, affecting at least 13 bird and seal species. (Science)
- Milk production in infected cows lasts about 60 days and costs nearly $1000 per affected cow. (CIDRAP)
Measles News:
- Measles is the highest it’s been in Europe for 25 years, the WHO says. (BBC)
- Vermont has its first measles case this year, in a child returning from international travel. (Vermont Health)
- Infants are at higher risk of complications from the measles but can’t be vaccinated right away, so parents near outbreaks have a painful waiting period. (NY Times)
- Texas’s lack of rural health infrastructure is complicating the response to the measles outbreak there. 64 TX counties don’t have a hospital, and 25 lack primary care physicians. (TX Tribune)
- The Mountain West may be at higher risk for a measles outbreak due to a low vaccination rate of just under 90%. (WPM)
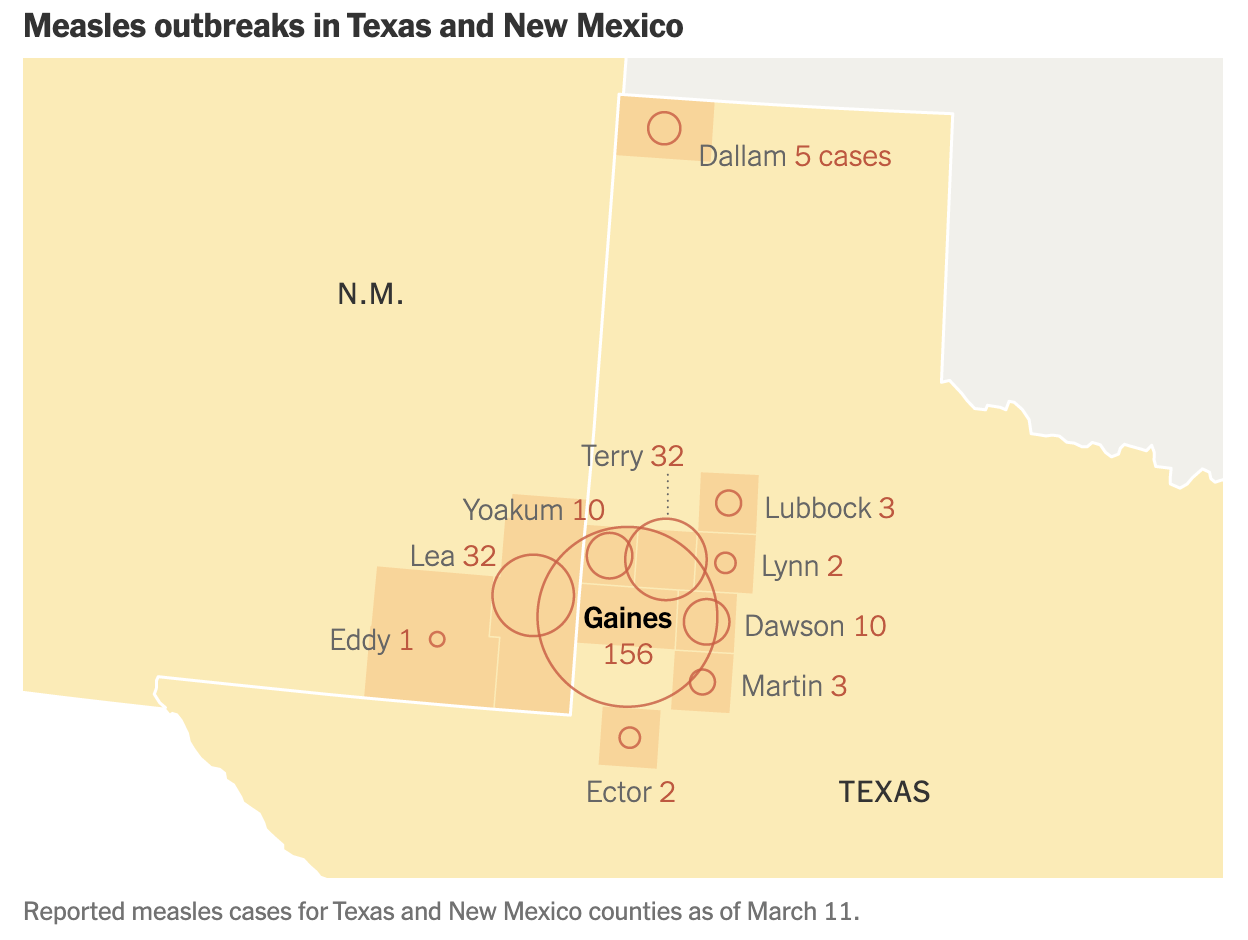
- This map from the NYT shows where cases were as of Tuesday. Since then, confirmed TX cases are up by 36, to a total of 259 as of Friday. (TX DSHS, NYT)
Health News:
- After cancelling its meeting of independent advisors, the FDA issued 2025-26 flu recommendations following WHO recommendations. (CNN)
- Most in the medical community now consider COVID endemic, meaning it’s regularly occurring, like the flu. It’s more transmissible, though, and there will still be waves and deaths. (Washington Post)
- Americans’ views of their mental and physical health are at the lowest point in nearly 25 years, according to a new Gallup poll. (Hill)
- COVID vaccines have paved the way for cancer vaccines. (WIRED)
- …but after the NIH cut funding for research on vaccine hesitancy, mRNA vaccine research might be next. The acting Director requested info last week about funding for mRNA vaccine research. (NPR)
Best Questions:
An employee was exposed to someone with measles. Can they work?
If an employee is exposed to someone with measles, the local health department usually tells them that they can’t work until they provide proof of vaccination. Both TX and NM, where the current U.S. outbreak is centered, require two doses of MMR vaccine for kids before they enter kindergarten and have for decades. So, unless an employee received an exemption as a child, if they went to public school, they’re probably vaccinated, but they’ll need to find proof. They can start by asking their family or caregiver, calling their childhood pediatrician, or checking to see if their vaccination records are available online through a state registry. They should call their doctor by phone for guidance if they’re not sure if they’re vaccinated. If they can’t prove that they’ve been vaccinated, they will generally need to stay out for 21 days from their date of exposure to ensure they’re not spreading the virus. In many cases, if they get a dose of MMR vaccine within 72 hours of exposure, they may be able to return to work sooner. You should always defer to the local health department in measles exposure cases. If you have an exposed employee and haven’t been contacted by your health department yet, you should be prepared for a surprise visit.
Source: CDC
An employee has backyard chickens. Should we be worried about bird flu?
While most humans are at very low risk for getting bird flu, there is an elevated risk for people who have close contact with birds, including backyard poultry flocks. There have been very few human cases in the U.S. outside of dairy workers and those culling infected birds at commercial poultry farms. But the person who died in Louisiana primarily had contact with their sick backyard chickens, so it’s certainly possible for a person to get sick if their birds do. That said, there haven’t been any cases of human-to-human transmission, so even in the very rare circumstance that an employee were to get sick, there’s really a very low risk of any kind of outbreak situation right now. If you do have an employee with backyard chickens or one who works with poultry or dairy cows, it’s important that they know of the risks and symptoms. If they have sick or dead birds, they should take careful precautions and wear PPE before entering the coop or touching animals. CDC has good guidelines here. They should be on the lookout for symptoms as well; pink eye is most common, but some cases might have flu-like symptoms, too. If an employee has symptoms of pink eye, we recommend excluding them for at least 24 hours, but if they mention that they have sick or dead backyard chickens, they should go get tested for flu and mention it to their healthcare provider. Again, there’s been no human-to-human spread, so this is a very low-risk situation. If you have an employee test positive for H5 type flu, don’t hesitate to reach out to ZHH. We can help work with your food safety, comms, and PR teams to liaise with the local and state health departments.
Sources: KFF Health News, CDC
Best Read:
One of the most interesting developments to come out of the COVID pandemic is the rise of wastewater testing, and the potential it has to stop the next pandemic in its tracks.
How disease detectives are hunting for viruses at major U.S. airports - CBS News